Tracking lost revenue and staying on top of fee schedules and insurance co-pays is more important than ever. Analyzing data from insurance plans, procedure payments, and fees can help you better monitor your managed care insurance plans.
The Utilization Report can help you monitor co-payments versus your clinic’s regular fees and identify insurance carriers with low coverages. You can customize the report to review insurance carriers and filter by date, procedure type, clinic, and provider, among other options.
After you have customized the report settings, you can then save the settings as the default for future use.
To generate the Utilization Report:
- Click the DXOne Reporting button on the toolbar
 , select Ledger, and then double-click Utilization.
, select Ledger, and then double-click Utilization.
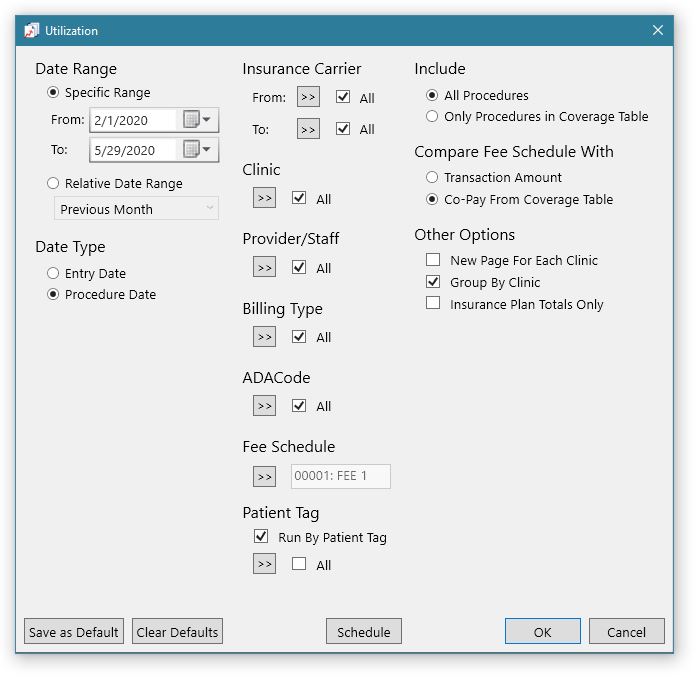
- Select your options, and click Save as Default to save the settings as the default report template. If needed, you can click Clear Defaults to reset the options back to the original default settings.
- Under the Compare Fee Schedule With section, you can select Transaction Amount to show only the fees that are attached to the procedure or Co-Pay From Coverage Table to show the fee attached to the procedure posted in the Ledger.
- Review the options you selected, and click OK to preview the report.
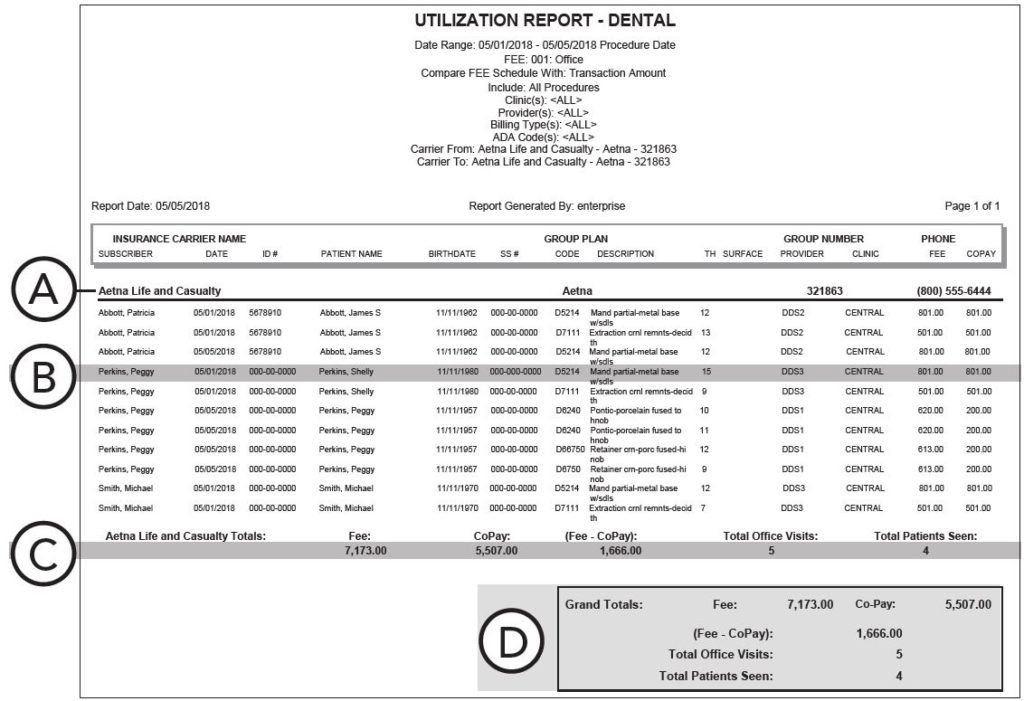
A. Lists the insurance carrier name, group plan name and number, and phone number.
B. Lists the patient’s name and the procedure posted in the Ledger (if the Insurance Plan Totals Only checkbox was not selected in the report options).
C. Lists the total fees, co-pays, office visits, and number of patients seen.
D. Shows the grand totals of fees and co-pays. Also, (Fee – CoPay) is the total revenue that would have been gained or lost had the fee schedule you selected in the report options been used when posting the procedure(s), total office visits, and total patients seen.
- Print or export the report from the Report Preview window.
Note: The Utilization report is not historical. If, for example, the insurance carrier changed for a patient, the reportable procedures would be populated for the “current carrier,” not necessarily the carrier in place at the time of service.
Additional Information
- You can schedule the report to run automatically on a date and time you set. To read more about how to schedule reports, see the Scheduling report jobs Help topic.
- For more information, see the Utilization Report Help topic.
- For more information on this report, see the Utilization Report section of the Dentrix Enterprise 11.0.2 Reports Reference guide in the Knowledgebase in the Dentrix Enterprise Resource Center. Both the Knowledgebase and the Dentrix Enterprise Essentials Training Videos are included with your Dentrix Enterprise Customer Service Plan.