Over time, your clinic may be saddled with unpaid insurance claims, which can fill up your insurance claims reports. Posting write-offs and zero payments on each claim individually can take up your staff’s time.
With Dentrix Enterprise 11.0.2, you can use the new Outstanding Claims Manager to identify and close outstanding claims that do not have any associated insurance payments. You can close multiple claims at one time rather than individually.
How to Process Unpaid Claims
1. In the Office Manager, from the File menu, click Outstanding Claim Manager. Or, click the Outstanding Claim Manager button ![]() on the toolbar. The Outstanding Claim Manager opens.
on the toolbar. The Outstanding Claim Manager opens.
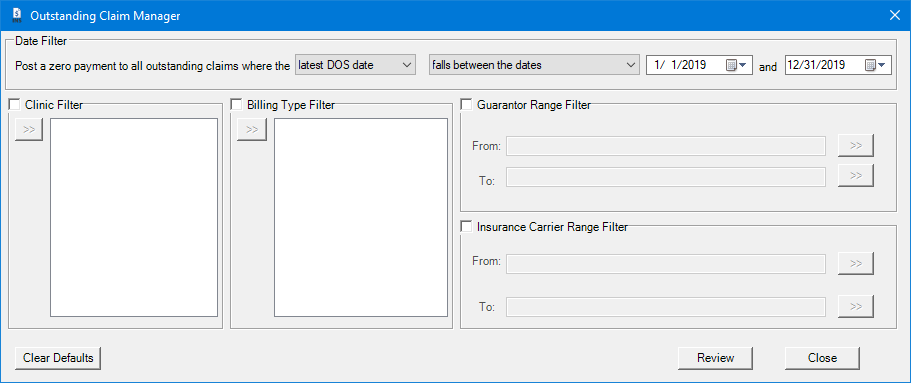
2. In the Outstanding Claims Manager dialog box, use the filters to identify the claims you want to review. For example, you can create a filter to only show claims by a certain claim creation date, by billing type, by clinic, and insurance carrier.
Notes:
- If you have made any changes to the filters, and you attempt to close the Outstanding Claim Manager, a message that asks if you want to save the new filters appears.
- If you want to reset the filters to the default states, click Clear Defaults.
3. Click Review. The Outstanding Claim Manager – Review and Process dialog box appears.
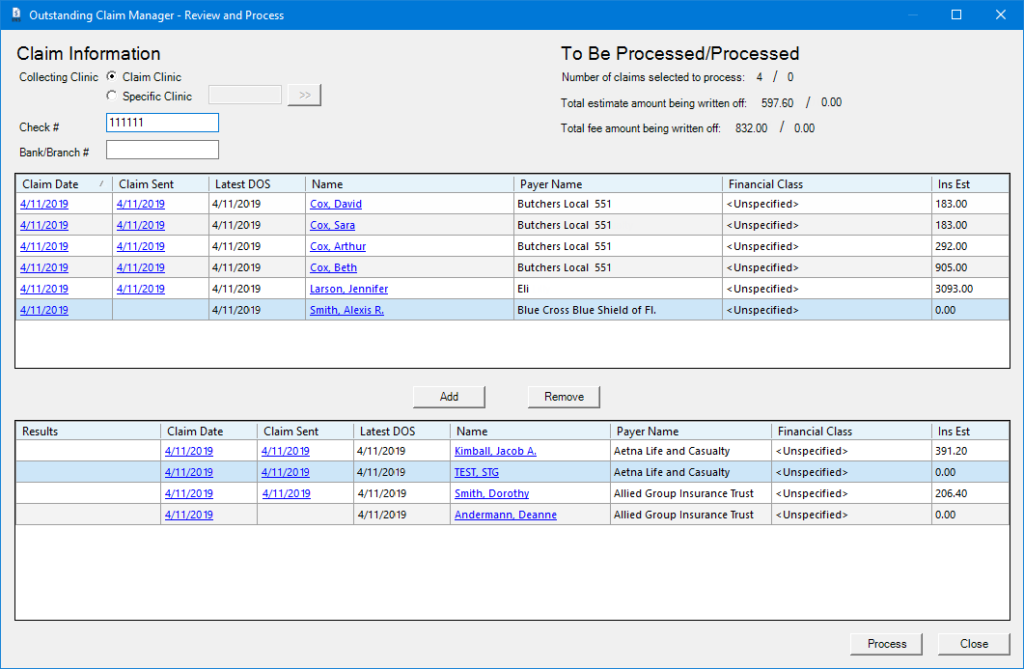
4. In the Outstanding Claim Manager – Review and Process dialog box, under Claim Information, enter the following information for the insurance payment:
- Leave Claim Clinic selected; or to switch clinics, select Specific Clinic, and search for your clinic.
- If applicable, enter the check number.
- If available, enter the bank or branch number of your clinic’s bank.
5. Select each claim you want to process, and click Add to move it to the bottom list.
6. When all desired claims have been added to the lower list, click Process. All processed claims will show a green Processed label.
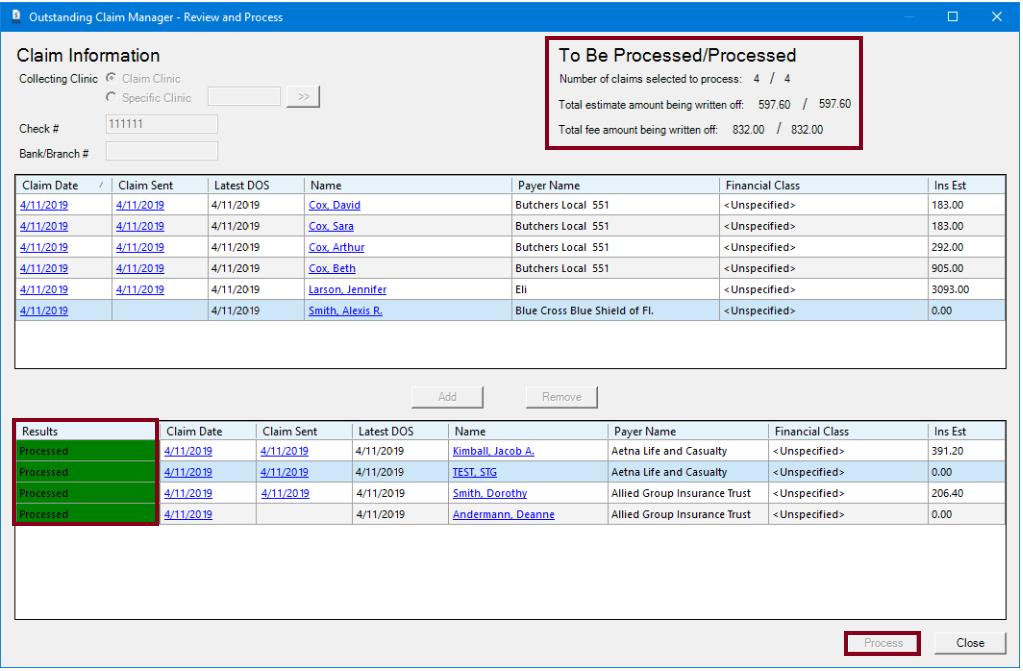
In the upper-right corner, a summary of the claims to be processed, total estimated amount being written off, and total fee amount being written off appear for your reference.
Note: When the outstanding claims are processed, they will no longer appear on reports such as the Insurance Claims Aging report.
Additional Information
- View the Outstanding Claim Manager Help topic to learn more.